Healthcare Oversight Commission Failure in Oslo: Manipulation and Deception
Health employees in Oslo use intimidation tactics and thuggery.
Date of event: 11 September 2025
Time of event: 10:30 AM
Location of event: Diakonhjemmet Hospital, Oslo, Norway
Oslo Health Authorities Attempt to Cover Up Abuses with the Help of Oslo Police.
At 09:21 a.m. on January 15, 2026, the journalist received a phone call from the Oslo Police, within a communication context linked to the health authorities. The call occurred amid broader circumstances whose indicators point to repeated attempts to pressure journalistic work and obstruct the publication of information concerning documented violations.
The timing and content of the call suggest an effort to deter publication and restrict public access to information grounded in documents and evidence of public interest. These actions appear to form part of an ongoing attempt by the health authorities to contain the truth and prevent its disclosure, following the forced admission trap case. These are matters the health authorities in Oslo declined to investigate, and in which the Oslo Police likewise refrained from opening any independent and impartial investigation, whether into these incidents or other related cases, revealing a pattern in which institutional loyalty appears to prevail over legal responsibility.
15.01.2026, Norway
The Role of the Police in Oslo: Legal Authority Absent from the Core of Law
In this context, the role of the Oslo Police cannot be reduced to individual conduct in the field, but must be understood as the outcome of structural distortions within legal and institutional decision-making mechanisms. Despite explicit guidance from an official at the Norwegian Ministry of Health to refer the incidents to the police, and despite assessments by health organizations identifying the acts as potentially criminal, the report was closed without any genuine investigation. The case was then redirected in a manner that reframed the doctor as the affected party, effectively shielding him from legal accountability.
This outcome does not reflect failures at the level of patrol officers or initial communications, but rather decisions taken within legal and administrative units, particularly legal affairs and internal prosecution. It forms part of a broader institutional pattern marked by the dismissal of sensitive cases and the selective application of the law, governed by internal loyalties rather than the rule of law. Compared to other Norwegian cities, where similar cases might trigger thorough investigations, the Oslo Police’s handling demonstrates a stark divergence from standard accountability practices.
Despite the photoshopped media image of the Oslo Police, recurring incidents expose a deeper structural failure. The issue is not a lack of authority or operational competence, but the absence of institutional will to hold the influential leadership within the security and institutional apparatus accountable. At the decision-making level, the law ceases to function as an instrument of justice and becomes an ethically eroded bureaucratic shield, used to deflect accountability, protect internal power balances, and normalize discriminatory and coercive practices.
This pattern cannot be separated from a long-standing institutional record in which cases have been handled according to personal and political interests for decades, with some violations only coming to light many years later. In this context, well-known cases such as Eirik Jensen are not cited as concluded criminal events, but as precedents revealing the vulnerability of the Oslo Police to internal corruption and the failure of oversight mechanisms to intervene before systemic dysfunction reached extreme levels. The Oslo Police has also been repeatedly linked to negligence or collusion with parties involved in serious legal violations both inside and outside Norway, including human trafficking cases, which have become subjects of international scrutiny. This reflects a significant gap between official statements on the rule of law and its actual enforcement.
The institutional logic can be summarized as follows:
Holding the doctor or responsible officials accountable necessarily entails holding the Health, Care, and Social Services staff at the County Governor in Oslo accountable for granting procedural cover and violating health rights, an outcome that is politically and administratively impossible.
Accordingly, the redirection of accountability is not discretionary but structurally inevitable. Here, the law operates to preserve institutional equilibrium, not to deliver justice or redress to the affected.
Beautification of the Report for the Formal Committee: A Mechanism to Conceal Violations and Manipulate Facts
When the case reached the Control Commission, the objective was not to hold the hospital accountable or investigate the violations, but rather to contain the scandal and give it a formal, seemingly independent façade. From the outset, it was clear that the oversight process was not objective, but a bureaucratic procedure designed to polish the external narrative while leaving the actual abuses unaddressed.
The chair of the commission, Elisabeth Grøndahl, demonstrated from the beginning a clear avoidance of her supervisory responsibilities, repeatedly excusing herself in every communication by saying she “was at the airport.” During the meeting itself, it became evident that she was prepared to interrupt and terminate the session. The focus was on presenting a linguistically edited report, rather than discussing the original report, which contained grossly unprofessional expressions, shocking contradictions, and undocumented allegations. This revision was purely formal, intended to mask the real motives and to avoid addressing the violations.
A Doctor Without Connection: A Symbolic Alibi Used to Cover Up Violations and Shift Responsibility
The leadership of the psychiatric department at Diakonhjemmet Sykehus brought in a doctor with an immigrant background, an uncommon occurrence in this department. The doctor was used as a front figure to present a new report. The purpose of this report was not to provide an independent medical assessment but to lend an appearance of legitimacy to a document that had already been prepared, shifting responsibility onto someone who had no knowledge of the case.
During the meeting, after the doctor realized that the case was suspicious and contained multiple irregularities, he openly admitted that he:
had no knowledge of the events,
had never met the affected person,
had performed no clinical assessment.
had written the report based on instructions from the hospital administration.
This development transforms the report into an administrative document supporting decisions that were already made, rather than an objective medical evaluation.
The question that cannot be ignored:
Why was a doctor, who has no connection to the case, involved as the face for preparing a report that lacks scientific basis, is biased, and lacks credibility, and is incapable of assessing the actual circumstances? How can such a report be considered reliable or objective, while the medical team hid and refused to confront the affected individual after carrying out the forced detention and preparing their retaliatory reports?
What took place within the framework of the health authorities in Oslo between 2022 and 2025 reveals a series of systematic, concerning, and unprofessional practices. Some healthcare institutions, which are originally meant to be bodies for care and treatment, and to operate in accordance with the law, medical ethics, human dignity, the principle of non maleficence, informed consent requirements, and remain independent of personal loyalties, were in certain cases transformed into tools with an authoritarian character. They were used for punishment and revenge instead of treating patients, raising serious questions about how medical power is exercised and where its limits lie. In some incidents, loyalty to responsible individuals appeared more important than legal and professional considerations, painting a troubling picture of authorities meant to protect citizens, not persecute them.
It is difficult to imagine the execution of such actions by health professionals municipal authorities or hospitals without some form of incitement institutional cover or implicit support from supervisory bodies This highlights a structural failure in accountability mechanisms and underscores the need for genuine independent oversight to ensure that medical authority is exercised responsibly rather than selectively
What is the scientific or ethical value of a report described as medical when it is completely detached from medical and humanitarian principles written in language that reflects no commitment to ethical standards and issued by an institution surrounded by a problematic record of criticized practices and violations
How reliable are diagnoses or assessments that shift from clinical tools into accusatory documents in which a therapeutic approach is replaced by the criminalization of legitimate criticism and in which pathological descriptions are used to undermine the work of journalists or silence individuals accompanied by repeated insinuations based on identity or ethnic and cultural background rather than actual health condition in a dangerous slide that links freedom of expression to medical stigmatization
When medical reports contain unethical comments retaliatory accusations and claims unsupported by established facts and the document turns from a scientific instrument into an authoritarian means of pressure or indirect threat aimed at obscuring the truth it becomes legitimate to question whether the assessment has completely departed from its scientific ethical and medical path and transformed into an administrative control tool disguised in false professional language
How can one trust a medical team that evades responsibility avoids meeting affected citizens or supervisory bodies and shields itself behind administrative offices instead of bearing the consequences of its decisions And how can such a team be taken seriously when it shifts responsibility onto a physician with no direct connection to the case in what appears to be a transparent attempt to avoid an open and uncomfortable confrontation
Health institutions founded on trust and integrity cannot tolerate such deviations without conducting deep and independent reviews that ensure the safety of the medical process protect individual rights and prevent the health sector from sliding into a tool for settling scores or silencing critical voices
When health institutions and senior authorities in Oslo become part of an escalation process and a system created to protect patients is used in certain cases as a means of pressure an administrative pattern emerges reminiscent of closed networks that exploit their authority to silence critics undermine public credibility and conceal the truth behind formal procedures
Instead of opening a full and objective investigation into the alleged violations some senior supervisory bodies participated in actions that can be interpreted as escalatory perhaps due to misjudgment or an unbalanced reliance on a single narrative in a manner suggesting the granting of a green light for actions that had previously been subject to review or doubt
The health authorities in Oslo municipality, from the municipal doctor through the administration and emergency preparedness leadership to Diakonhjemmet Hospital, which had previously acknowledged mistakes and sought to correct them, were suddenly given a green light. Today, these actors are the ones signing formal decisions of a retaliatory nature, supported by signals from the health authorities at county governor health authority (Statsforvalteren), clarifying the course of events and revealing which bodies were responsible for transforming systemic failures into institutionalized retaliatory decisions.
Decisions are often made quickly and decisively particularly when confronting cases involving documented violations by a physician who exploited weaknesses in the complaint system of the State Administrator in Oslo while the same standards are absent when addressing complaints submitted by affected citizens
Although supervisory bodies publicly assert that their role is to protect patients investigate complaints and strengthen public trust the facts presented raise serious questions about the extent of actual adherence to these principles and whether they are applied equally or selectively
These developments reflect a different reality and raise fundamental questions
Did the authorities fulfill their true role
Were complaints handled with seriousness or was disproportionate weight given to the narrative of a physician who claims that all his patients are lying while he himself falsifies assessments and who was granted a green light for further violations through documents of pressure and coercion aimed at submission and silencing
Were the decisions and responses consistent with general principles applied to all or were there indications of selective enforcement of rules.
The available official documents including correspondence letters and responses both published and unpublished show that the citizen presented evidence recordings messages and precise dates while the opposing party chose denial or disregard and avoided assuming responsibility in written communications As a result the situation escalated and took dangerous directions indicating that the citizen was subjected to incitement to violence against him sedation and forced transfer in a context that can be understood as an attempt to silence and intimidate him.
These events exposed patterns in the use of authority that exceed its lawful function and revealed clear structural deficiencies in investigation and accountability mechanisms since 2022 The use of involuntary commitment force and the misuse of personal identity and medical records along with the instrumentalization of ethnic or cultural background insinuations as means of pressure cannot be understood as individual failures but as indicators of a deep institutional malfunction within the oversight system This case is not an isolated incident but a serious warning of eroding procedural safeguards the absence of genuine independent oversight and the resulting risks to transparency accountability and the protection of rights and freedoms in Oslo.


"The events that took place during the meeting of the control commission reveal the need to establish an independent committee to investigate manipulation and bias, in order to ensure integrity and transparency in the processes."
In a broader context: Abuse of medical authority as a punitive tool
What is revealed here shows an institutional pattern:
medical reports are written in advance without clinical basis,
coercion is used without medical necessity,
closed patient records are reopened by involved staff,
and oversight processes are manipulated to prevent accountability.
This aligns with the international concept of “Punitive Psychiatry,” where psychiatry is used for pressure and sanctioning, not treatment.
Analytical summary
The material exposes a closed system that operates through self-protective mechanisms rather than accountability.
Oversight committees are used as formal shells to legitimize predetermined decisions.
Psychiatry is used as a tool of intimidation rather than a treatment method based on science and ethics.
Lawyers and supervisory bodies are misled or excluded to prevent access to information.
Those truly responsible hide behind administrative facades without consequences.
This undermines trust in the health and legal systems in Oslo and clearly shows the need for an independent and comprehensive review.
To understand the gravity of the patterns revealed in this case, it is necessary to view them in light of historical experiences with the abuse of psychiatry as an instrument of power.
History shows that the abuse of medical authority to label individuals as “mentally ill” for unprofessional or political purposes is not a new phenomenon. As has also been demonstrated in this case, numerous historical experiences show that psychiatry has, over time, been used as a tool to suppress and delegitimize individuals.
In the former Soviet Union, the so called punitive psychiatric system was used to classify political dissidents as having “sluggish schizophrenia,” depriving them of their freedom and resulting in involuntary institutionalization without scientific basis. In Nazi Germany, psychiatric diagnoses were used to legitimize the T4 program, which involved forced sterilizations, mistreatment, and in many cases the killing of thousands of individuals deemed to have “unworthy lives.”
Misleading the Lawyers: An Attempt to Conceal the Outcome of the Meeting
After the meeting, the commission chair, Elisabeth Grøndahl, carried out a series of actions that indicate deliberate manipulation. She refused to provide the meeting’s outcome to either the lawyers or the affected individual.
When the affected person called her, she claimed she did not remember the case, while at the same time admitting that the case had been decided in the hospital’s favor immediately after the meeting.
She then stated that the case had been sent directly to lawyer Erlend Liaklev Andersen.
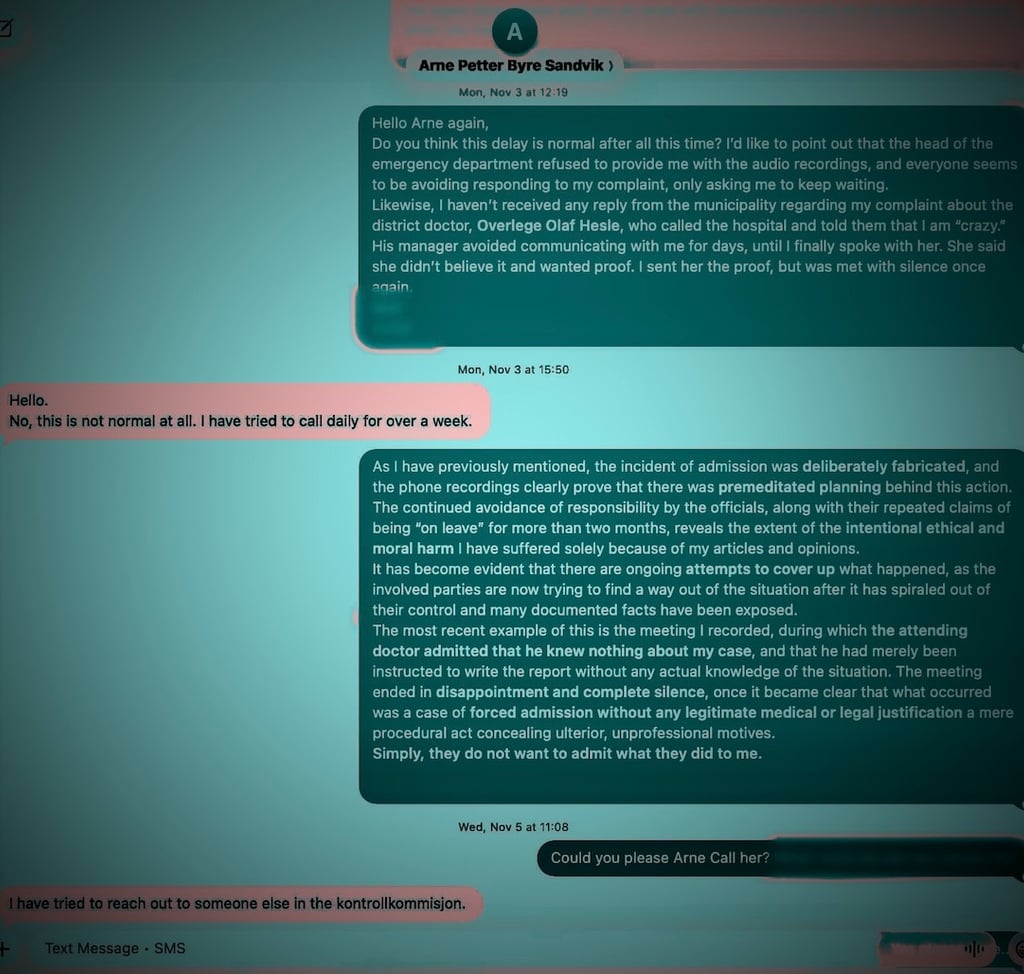
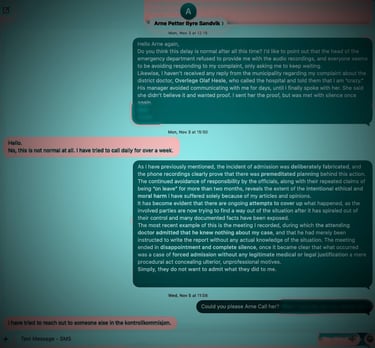
Lawyers Erlend Liaklev Andersen and Arne Petter Byre Sandvik were subsequently met with delays and silence, reflecting a clear unwillingness to ensure transparency or accountability. This is not an isolated incident, but part of a system that protects itself.
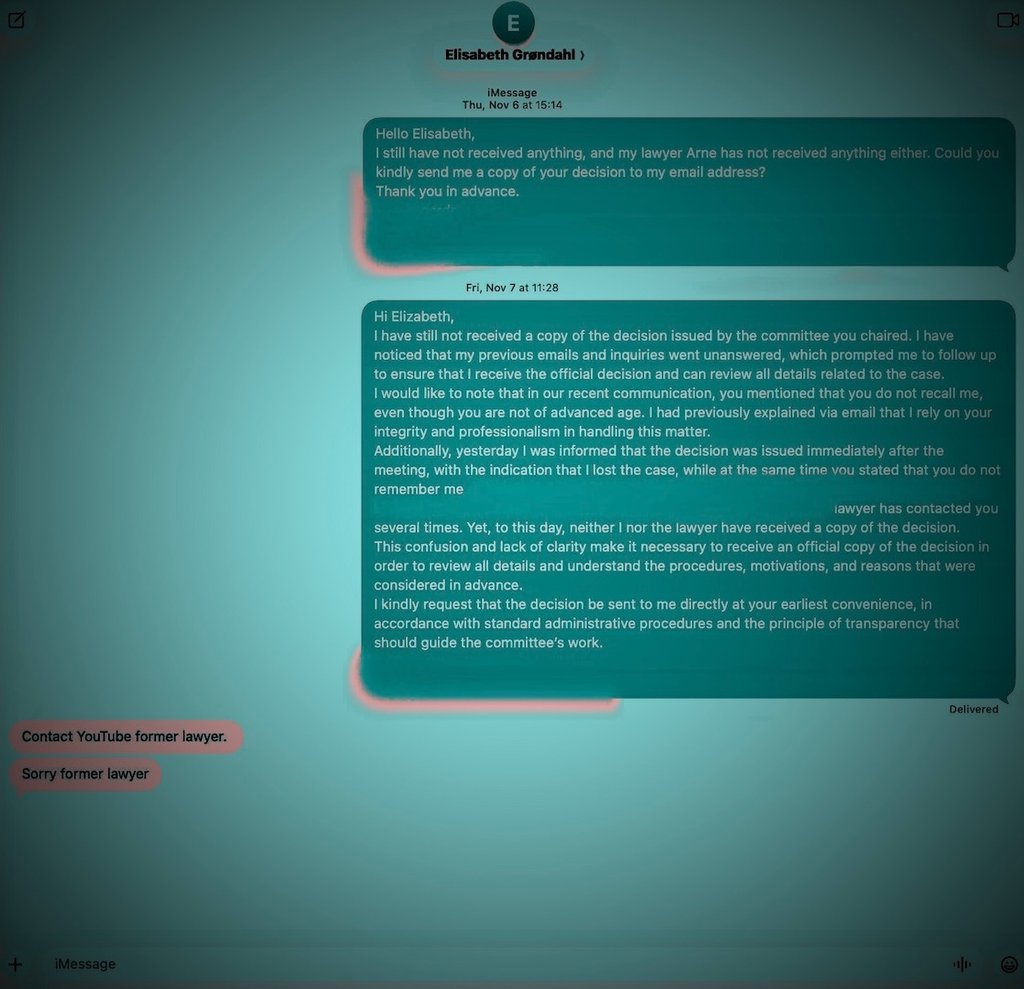
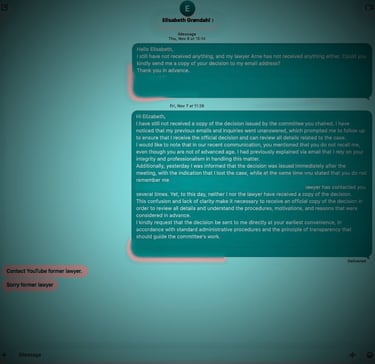

Through a phone call, the head of the Control Commission, Elisabeth Grøndahl, confirmed that the decision was delivered immediately after the committee meeting to lawyer Erlend Liaklev Andersen. Later, via SMS, Grøndahl informed the affected person to contact the relevant lawyer for updates.
These messages came after a series of repeated emails from the affected person, following unjustified silence, but Grøndahl failed to respond from the committee meeting date on September 11, 2025, until November 6, 2025, when a follow up message was sent after a deliberate delay.
This illustrates how difficult it is to achieve transparency and formal follow up from the commission.
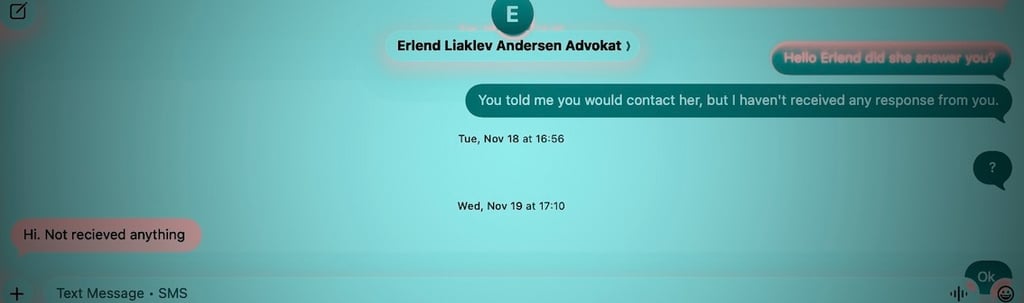
On November 19, 2025, lawyer Erlend Liaklev Andersen informed that he had not received any response or copy of the committee's decision, which clearly demonstrates ongoing difficulties in accessing official documents related to the case.
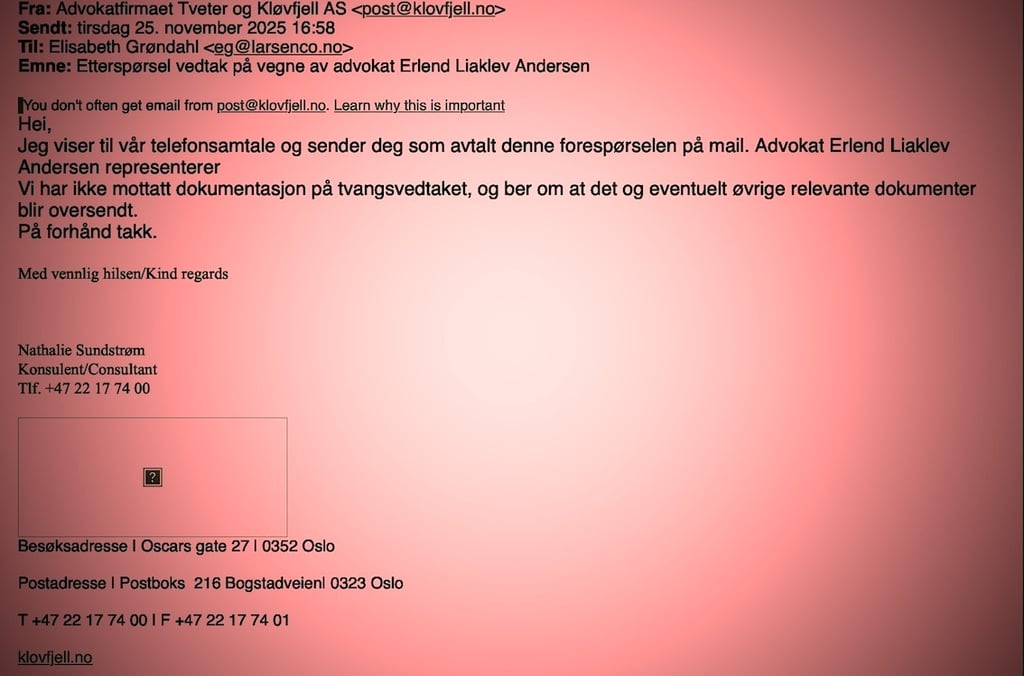
On November 25, 2025, lawyer Erlend Liaklev Andersen’s office contacted committee chair Elisabeth Grøndahl via email again to request any documents or a copy of the committee’s decision.
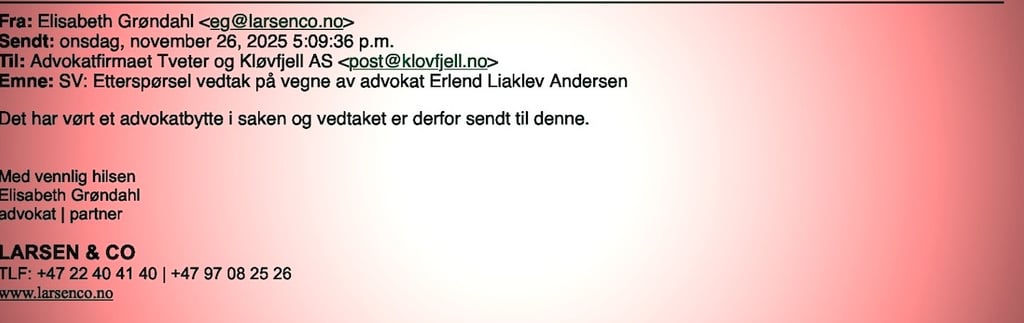
When the lawyer himself requested the decision that was claimed to have been delivered to him, the chair of the committee, Elisabeth Grøndahl, provided neither a copy nor any clarification. Instead, she responded with an evasive and misleading statement, referring to a “change of lawyer in the case” and asserting that the decision had therefore been sent elsewhere, without specifying to whom and without providing any documentation.
Through this ambiguous and contradictory response, all parties were misled simultaneously, and the final outcome was identical: Neither any lawyer nor the affected individual received any formal decision.
This pattern of systematic evasion and conflicting explanations does not appear accidental, but raises serious questions as to whether the course of events formed part of a coordinated process, enabled or supported by higher health authorities, rather than corrected or halted.
The committee chair has refused to communicate with the lawyers or to provide any documents related to the case. This is clearly demonstrated through the repeated attempts made by attorney Arne Petter Byre Sandvik, who tried multiple times to contact the committee without receiving any response. Even after attempting to reach other members of the Control Commission, it has proven extremely difficult to obtain access to official information.
Through a review of events, it becomes evident that the health authorities continue to employ the same methods against critics, by exploiting personal and medical information as a means of pressure through the traditional channels linked to medical records or the “medical journal.” These practices do not appear to be isolated incidents, but rather a recurring pattern.
The case officer in question, who previously granted the physician exclusive access to the patient’s medical record which was later used for coercion and defamation now presents as a neutral supervisory authority, despite having played a direct role in enabling these abuses. The measures appear lawful on paper, but in practice are used to silence critical voices and avoid genuine accountability.
This pattern raises fundamental questions about the limits of power, and about whether the legal framework is being used for protection and accountability, or as a pretext to legitimize pressure tactics that violate basic ethical principles in health governance.
Acknowledgment and Measures Implemented by Diakonhjemmet Hospital
On August 28, 2025, Diakonhjemmet Hospital acknowledged having reopened the medical record of the affected individual, which had previously been officially closed, providing justifications that are not legally defensible.
What is concerning is that this action did not occur in isolation; the timeline and available evidence suggest a certain level of support and insight from the highest health authorities at the County Governor’s office in Oslo. The reopening of the record occurred after complaints regarding the doctor who had influenced authorities were presented, and there was collaboration with the doctor to use the affected individual’s medical record as a tool of pressure to force silence and prevent documents and facts from being made public, while granting the doctor exclusive access to the record.
The incident exposes significant weaknesses in oversight, where the formal justifications provided a veneer of legitimacy, even though they did not address the actual violations. This makes responsibility shared between the hospital and the authorities that approved the action.
Exploitation and Legal Violations
The medical record that was reopened was used as a tool for data manipulation and pressure against the affected individual. This action was neither random nor unplanned, but resulted from measures supported by certain parties within the health system, raising serious questions about possible illegal coordination in decision making.




Advokat Erlend Liaklev Andersen
Attorney
Arne Petter Byre Sandvik
Attorney
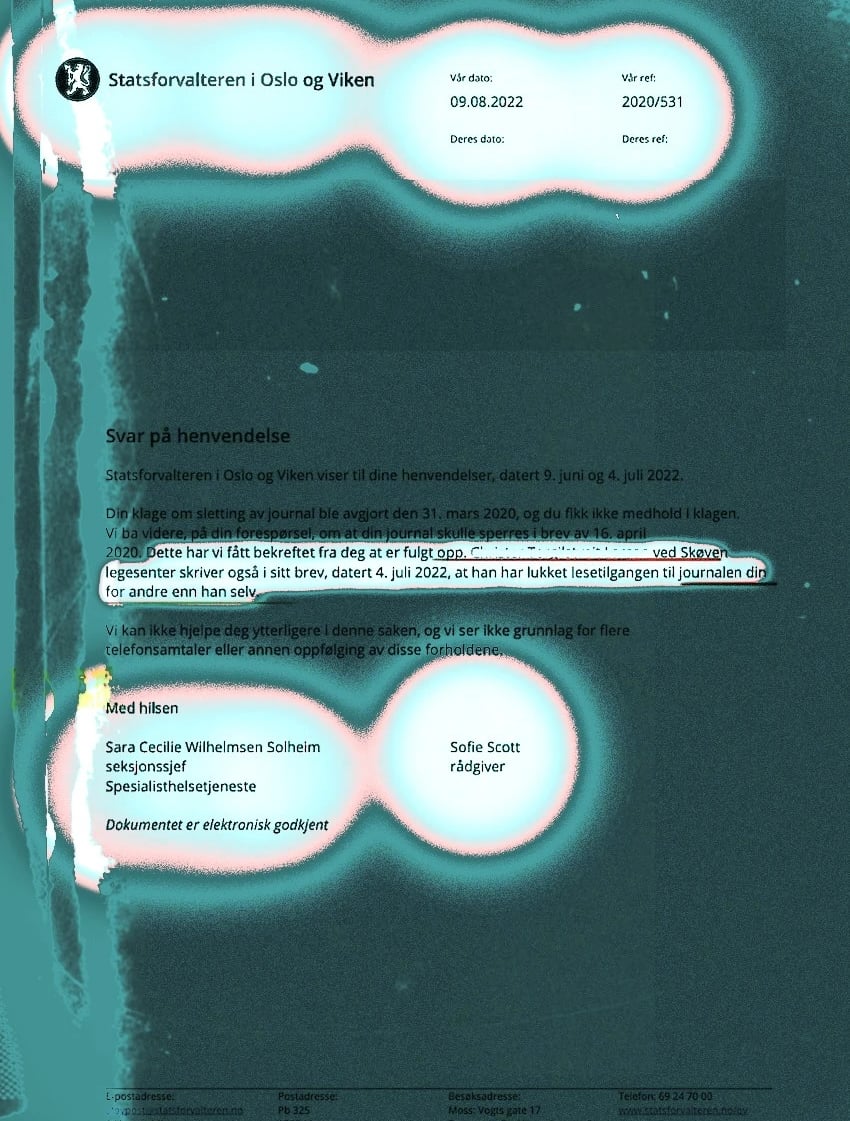
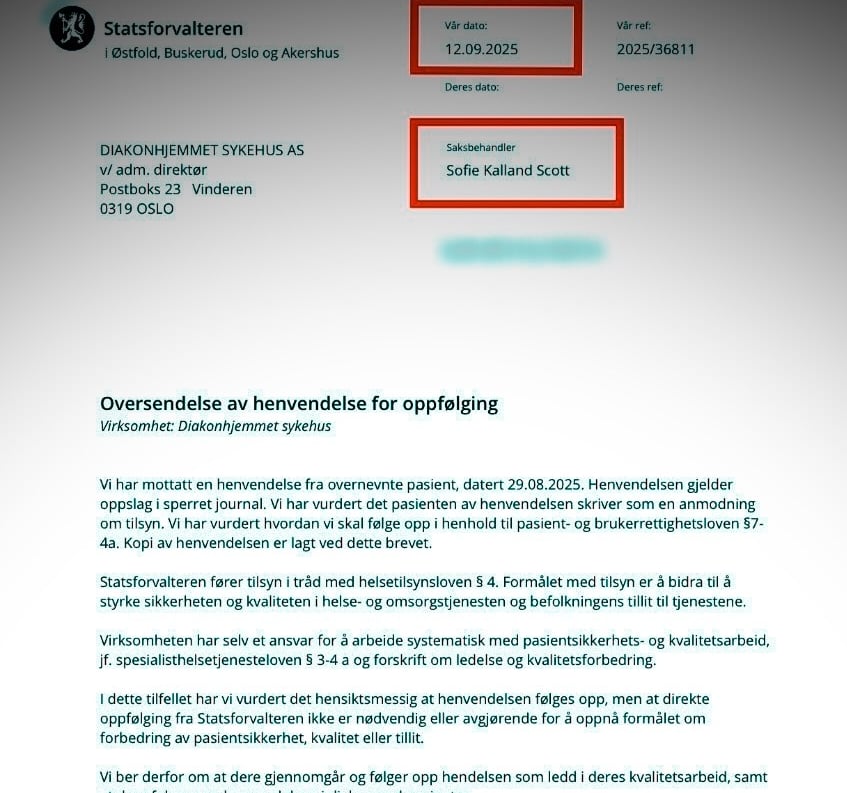
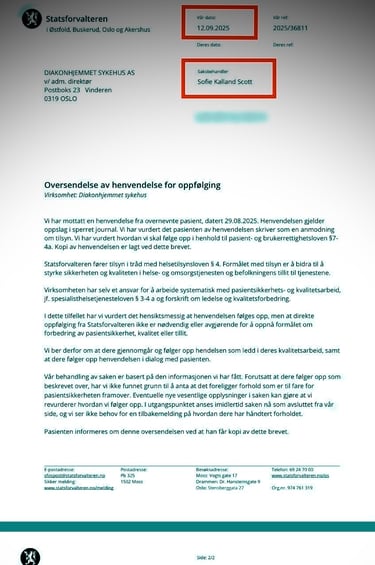
The 2022 decision, issued by Sofie Scott and Sara Cecilie Solheim, did not address the core of the complaint against the physician. Instead, the issue of medical records was shifted into a parallel procedural track that, in practice, functioned as a diversion from genuine accountability.
Rather than investigating documented and non-relevant manipulation, this track was used to justify closing the case, while simultaneously granting the physician discretionary authority that enabled the medical record to be used as a tool of pressure and subjugation.
The outcome was not the protection of the affected individual’s right to health care, but an institutional practice in which the medical record was instrumentalized to silence the case. This points beyond the weaknesses of a single decision and reveals a structural pattern in which the absence of effective oversight enabled subsequent repetition.
Role of the Case Handler
It is noteworthy that the case handler at the County Governor’s office in Oslo, who is the same person who prepared the formal document mentioned above, granted the involved doctor, who has been implicated in these violations since 2022, exclusive access to the medical record (09.08.2022 – 2020/531). This decision can be seen as an implicit approval of the breaches, as the record was used as a tool for pressure, manipulation, and defamation, with support from local authorities to enforce sanctions against the affected individual. This gave the controversial doctor the opportunity to escalate events in a dangerous manner.
Official Practices and Formal Procedures
When the complaint was submitted to the health administration at the County Governor’s office in Oslo, neither Diakonhjemmet Hospital nor any of the involved entities took any real steps to contact the affected individual or respond to the complaints raised. The responses that were given were formal and superficial, reflecting neither a thorough investigation nor a detailed handling of the case. Additionally, the measures and responses implemented did not include any actual law enforcement but appeared as formal procedures intended to give a supervisory impression without concrete action to resolve the matter.
Conclusions and Outcomes
This case raises serious questions about the role of health administration at the County Governor’s office in Oslo in ensuring the protection of the affected individual’s rights. While the official responses may have appeared to be provided in accordance with applicable law, the reality reveals a concerning lack of efficiency in processes and a lack of transparency in handling these sensitive matters. Furthermore, the hospital’s and health administration’s silence regarding the doctor’s role in incitement and defamation, as well as the absence of responses from the committee for involuntary admissions, raises suspicion of possible collusion among the involved parties.
"The situation is now so clear that it no longer requires Braille for some to understand or acknowledge it."
Dark chapters also exist in Scandinavia: in both Sweden and Denmark during the 20th century, extensive programs were carried out for the forced sterilization of individuals labeled as “mentally deficient” or “mentally ill.” These assessments were often based on social and political criteria rather than medical standards, with the aim of controlling the composition of society.
These historical examples demonstrate a clear pattern: when psychiatry deviates from its scientific principles, it can become a tool for power and revenge. The misuse of medical authority has historically led to deprivation of liberty, involuntary hospitalization, loss of civil rights, and in the worst cases, loss of life.
Historical experiences with the abuse of psychiatry as a political and social tool, as well as an authoritarian, oppressive, and intimidating instrument, provide a clear example of what can happen when medical authority deviates from scientific standards. Incidents that have occurred in Ullern, Frogner, Aker emergency clinic, Diakonhjemmet Hospital, and the Adult Psychiatric Department Vinderen in Oslo illustrate how a lack of integrity, transparency, and adherence to scientific principles in medical practice can harm individuals, restrict freedom, deprive rights, and impose unjustified coercive measures.
At the same time, amid neglect and silence from the health authorities, including the County Governor of Oslo, who has the overarching supervisory responsibility, the risk of individuals’ rights being disregarded increases. This demonstrates that the phenomenon is not merely theoretical or historical but has real consequences in today’s healthcare system in Oslo, underscoring the urgent need for effective oversight and strict enforcement of scientific, ethical, and legal standards in medical practice to ensure that medical authority is never used to harm people or undermine their rights.
Thus, the events themselves became clear evidence of the accuracy of what had previously been published; the health authorities’ use of involuntary hospitalization merely confirmed the documented abuses and serves as a living example of violations of patient rights and applicable laws in Oslo, where medical power is exercised without legal safeguards or independent oversight.


The Aktion T4 program is a historical warning of how medicine can be misused as an instrument of power without legal oversight.


Political prisoners in the Soviet Union were held in psychiatric institutions because of their oppositional views, a historical example of using psychiatric diagnosis as a tool of political repression rather than for health care.
This image represents the birth of the human rights movement in the Soviet Union, in response to the abuse of psychiatry as a tool for political repression. The persecution begins with the criminalization of opinions, followed by labeling them as a disease, and ends in forced confinement outside the boundaries of the law.




A psychiatric hospital in the Soviet era, where mental institutions were used as a tool to confine political dissidents under so called medical diagnoses.
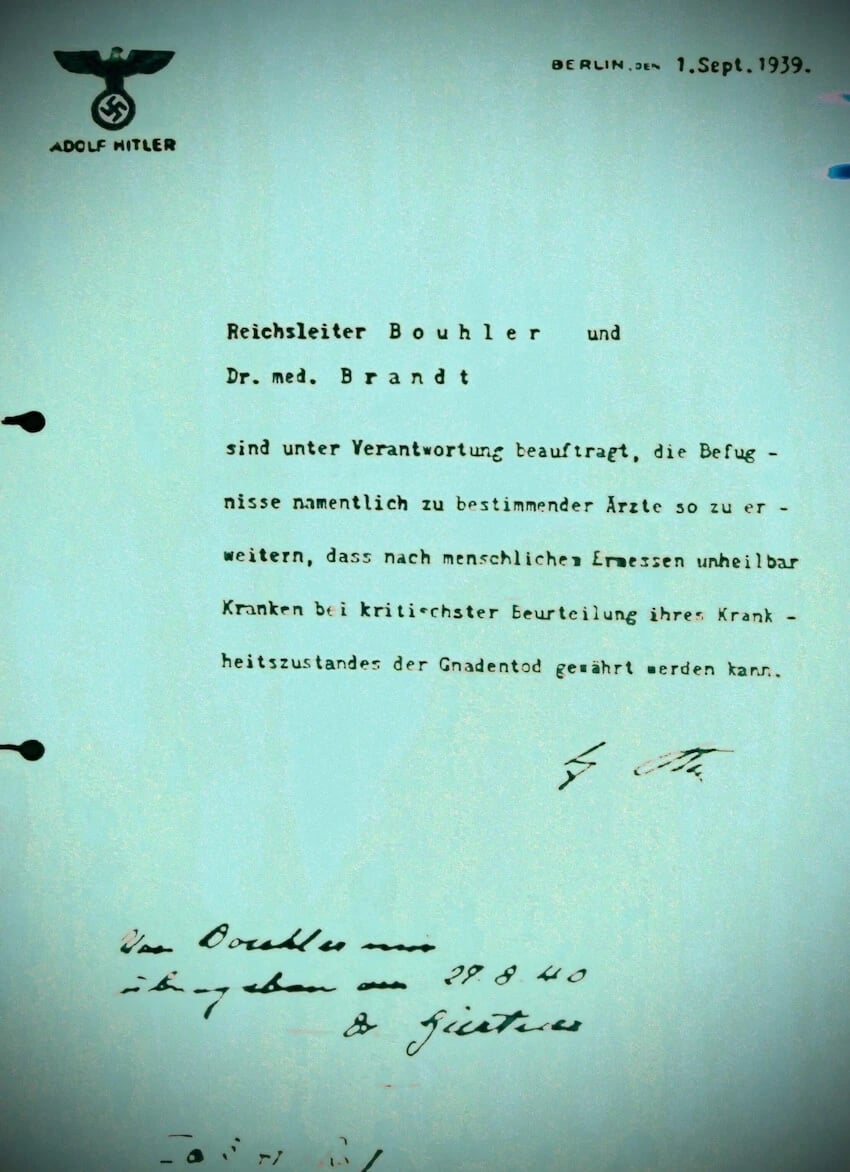
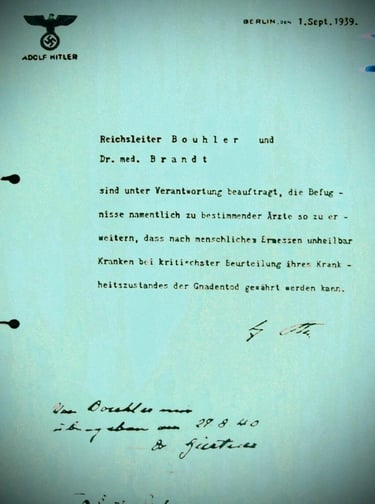
This document, dated 1 September 1939, represents a direct authorization from the highest political authority in Nazi Germany, granting designated physicians exceptional powers to make life and-death decisions concerning patients classified as “incurably ill,” based on subjective medical judgment. Its significance lies not only in its wording, but in its implication: the transformation of medical diagnosis into an instrument of power, stripping certain groups of legal protection in the absence of any independent scientific or judicial oversight. It stands as a stark historical example of how psychiatry and the medical establishment can be instrumentalized as mechanisms of control and repression rather than care and protection.
Testified on 05 December 2025
The documentation shows that the sequence of events escalated through the doctor in question, who took over the practice of the retired physician at Skøyen Health Center in 2022 and 2023. Documents and witness statements indicate that his administrative influence was used in a manner that created an atmosphere of pressure and intimidation, employing certain healthcare workers as instruments for improper influence, after reliable information emerged questioning the legality and safety of his professional conduct.
These circumstances reveal a complex background illustrating how abuse of medical authority can become an unethical tool that inflicts psychological, moral, and societal harm on patients. There have been reports of attempts to stigmatize certain patients with psychiatric labels that were not based on accurate medical assessments, as well as the preparation of reports with punitive or harassing content, which appear to be reactions to patients expressing facts or information that certain responsible parties did not want disclosed.
The documentation also shows deliberate attempts to threaten and silence journalists and critics who exposed or documented the abuses, including implicit threats and pressure intended to prevent publication and investigation, aiming to obstruct the emergence of the truth and protect the interests of certain authorities.
Documentation of this case also raises questions about the equal application of the law in Oslo, particularly with regard to patients with foreign backgrounds, where reports indicate discriminatory treatment that undermines their rights and human dignity. This suggests a potential pattern in which certain citizens are not recognized as full legal subjects, despite having the same legal rights as others, as stipulated by the Constitution regarding equality and the protection of all citizens’ fundamental rights.
Taken together, these issues raise fundamental questions about procedural safety, legal security, and the distinction between medical authority and individual rights, underscoring the need for an independent review to ensure that healthcare institutions are not used in practices outside their professional and humanitarian framework in Oslo.